Community-level interventions for people who can’t access conventional health services are key to getting ahead of the HIV epidemic
An HIV program in KwaZulu-Natal, South Africa, is among the first in the country to reach UNAIDS’s ambitious targets to test, treat, and suppress the viral load of 90 percent of people living with HIV, according to survey results released today at the South Africa AIDS Conference (SAAIDS) by the international medical humanitarian organization Doctors Without Borders/Medecins Sans Frontieres (MSF).
The survey of MSF’s community-based HIV/TB project in Eshowe, KwaZulu-Natal, showed that 90 percent of people living with HIV knew their status—of which 94 percent were on antiretroviral treatment and 95 percent had a suppressed viral load. Along with similar findings from several other HIV population surveys, including two surveys released at SAAIDS this week, the MSF results provide strong evidence that achieving the so-called 90-90-90 UN target (in which 90 percent of HIV-positive people know their status, 90 percent are on treatment, and 90 percent have a suppressed viral load) is possible in South Africa. The survey also revealed encouraging data suggesting that the number of new infections is decreasing in certain areas.
“We’ve shown that it’s possible to reach 90-90-90 in an area with one of the highest HIV infection rates in the country, where one in four people is living with HIV,” said Dr. Liesbet Ohler, MSF’s project medical referent in Eshowe. “These results are a testament to the full engagement of the entire community. Everyone—from local civil society and patient groups, health staff and traditional health practitioners, traditional leaders and their members—was deeply involved in designing and helping this project deliver from the beginning.”
The population-based survey presented at SAAIDS was conducted by Epicentre—MSF’s research arm—and included 3,286 people aged 15 to 59 years. The results were compared to the findings of a 2013 MSF Epicentre survey of 5,649 people aged 15 to 59 in the same area. Participants completed detailed questionnaires and had an HIV test done; if confirmed HIV-positive, further blood tests were taken to measure viral load and CD4 counts, which shows how well a person’s immune system is working.
The 2018 survey found a significant increase in overall HIV status awareness (14 percent increase) and in starting people on treatment (24 percent increase) between 2013 and 2018. Among men, there were striking increases in knowledge of HIV status (from 68 percent to 83 percent) and those who were on treatment (from 68 percent to 87 percent).
Preliminary HIV incidence results (i.e. the number of new cases) show a trend to decrease, from 1.2 percent in 2013 to 0.2 percent in 2018.
This is supported by survey findings that show that among the people surveyed, the proportion of people living with HIV who were virally suppressed increased from 56 percent in 2013 to 84 percent in 2018. Viral suppression means that antiretroviral treatment is successfully suppressing the amount of virus in a person’s blood, ensuring overall health and greatly reducing the chances of HIV transmission. These changes from 2013 to 2018 signify a dramatic reduction in the number of people with the potential to transmit HIV to others and suggests a potential to decrease new infections.
However, significant challenges remain among specific age groups, and MSF cautions against interpreting the survey results as an outright declaration of victory.
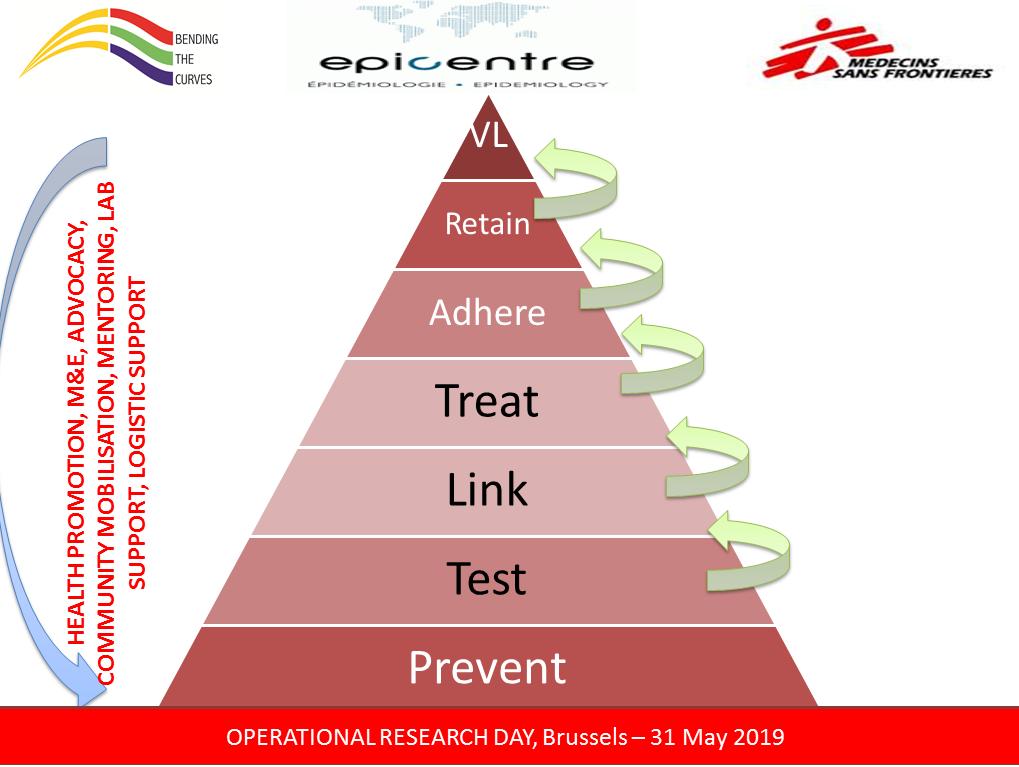
While incidence decreased among women aged 15 to 29 years, from 2.9 percent to 1.2 percent, this figure remains high and points to the continued risk faced by adolescent girls and young women. Difficulties also remain in reaching men, who overall achieve poorer treatment outcomes across what is known as the “cascade” of HIV care—which includes testing, links to treatment, treatment adherence, and viral suppression. More than half of young men aged 15 to 29 who are diagnosed with HIV are still not on treatment.
“We hope these findings will help focus our collective energies on reaching these groups who remain the most vulnerable to HIV,” said Dr. Laura Trivino, MSF’s medical coordinator for South Africa.
MSF’s “Bending the Curves” project—which started in 2011 before the 90-90-90 targets were set by UNAIDS in 2013—aimed to reduce the incidence of new HIV infections and HIV-related illness and death. Numerous activities were launched in partnership with communities and the KwaZulu-Natal Department of Health to prevent HIV infection, increase HIV testing, link people quickly to care, and support their adherence, retention, and suppression on treatment. Today the project covers 10 clinics and two hospitals. Early on, the project invested in community-based prevention and HIV testing strategies, including extensive door-to-door testing by lay workers, with over 120,000 door-to-door tests conducted between 2012 and 2018. Between 2015 and 2018, 1.35 million condoms were distributed annually.
“How did Eshowe get to 90-94-95?” said Musa Ndlovu, MSF’s deputy field coordinator in Eshowe. “I would say it’s the power of partnership. We had the total commitment of the traditional leadership, and close collaboration with the departments of Health and Education at each stage. In the early days of this project, it was almost impossible for people to even imagine talking about HIV. Today people even stop our MSF vehicles and ask for an HIV test. We didn’t do it for the community, we did it with them.”