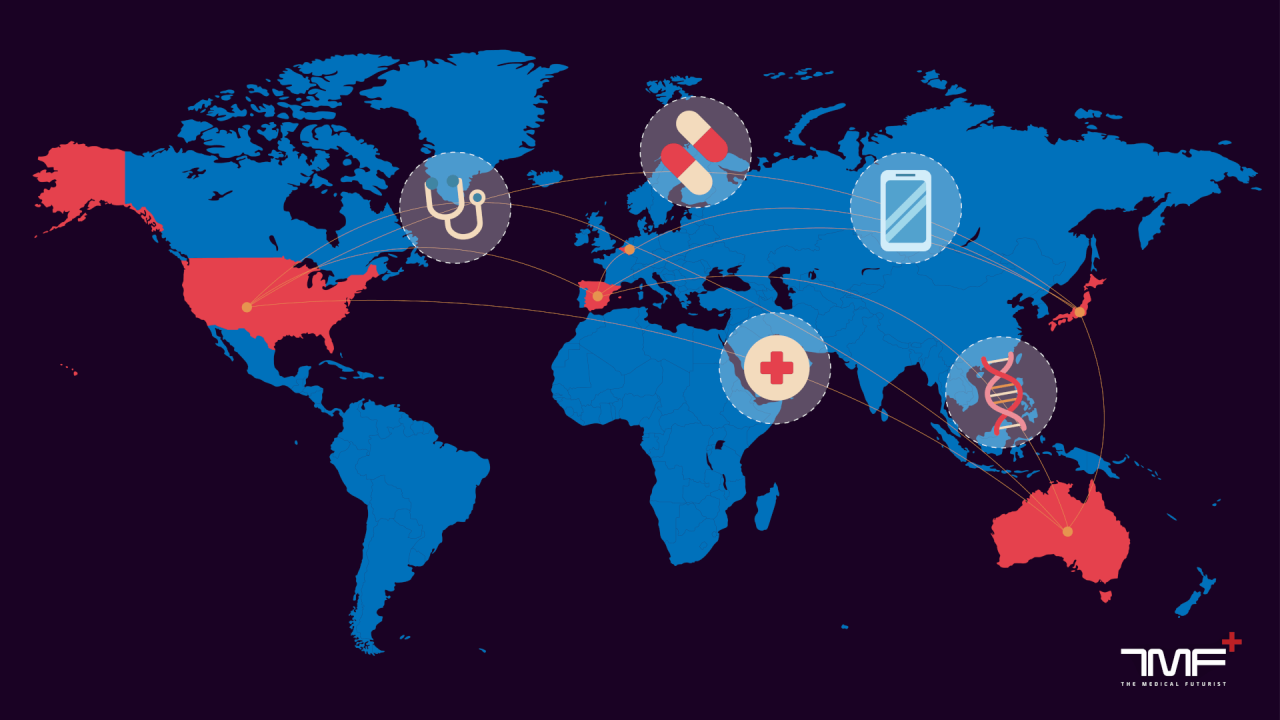
Digital Health makes Healthcare Globalised
Consider Atlas Biomed, the company behind the at-home microbiome test: it is based in the U.K. Some 1,900 kilometers away in Italy, Dante Labs offers direct-to-consumer whole genome sequencing kits. On the other side of the Atlantic Ocean, in the U. S., is Fitbit, which ships its fitness trackers around the world. Despite being headquartered in different countries and even in different continents, patients now have access to quality digital health services wherever they are (save for some shipping restrictions).
This aspect of digital health heralds one of its lesser-explored advantages: it enables healthcare to be truly globalised. However, more work has to be done as digital health moves towards this goal. From new regulations to updating physicians’ curriculum, policymakers will have to rethink the traditional healthcare landscape. But it’s not only policymakers but also stakeholders on every level of this landscape who will be impacted by this globalisation.
Join us as we dive into how digital health is grooming healthcare to be globalised and the steps needed to swerve this evolution in the right direction.
Digital health upends the healthcare market
The literature defines digital health as “the cultural transformation of how disruptive technologies that provide digital and objective data accessible to both caregivers and patients leads to an equal level doctor-patient relationship with shared decision-making and the democratisation of care”. The novel technologies that help in this cultural transformation help make patients the point-of-care with direct-to-consumer services.
This hasn’t been more apparent than with the COVID-19 pandemic. Prior to this crisis, only 1 in 10 U.S. patients used telemedicine services, a J.D. Power survey found. Now, due to the current circumstances, the use of some telemedicine apps has gone up by 158% since January. Cancer patients are continuing their treatment thanks to the technology. The FDA cleared Pixel by LabCorp’s at-home COVID-19 testing kit.
Demand for wellness apps and fitness wearables surged under the current circumstances. Even seniors are embracing health tech during the pandemic. And all of these services are available from the comfort of one’s home, even if the company is itself located elsewhere. By extrapolating these trends, it’s not far-fetched to imagine the following healthcare journey of a patient in the near future. Let’s visualise it.
Upon recommendation from their physician, a patient submits a cancerous tissue biopsy to a Belgian startup that can sequence its genome, as the technology is not available locally. The startup matches the genome to driver mutations in clinical trials whose database is in the cloud in the U.S. For an extra fee, the Belgian startup connects the patient to the clinical trial taking place in Spain; run by a French pharma company. The patient enrols in the trial and follows the treatment in Spain, subsidised by the pharma company.
While only the initial steps include a cost, the end result is that the patient ultimately receives state-of-the-art, targeted treatment for free. Without such a globalised network and accessibility to these services, the patient might not have had a chance at treating her ailment. This is the democratisation and globalisation of healthcare that digital health brings along. Even if this theoretical scenario sounds optimistic, such an approach is already possible in practice.
Meet the patient of the future
As The Medical Futurist, Dr. Meskó tries to live like the patient of the future. The data he brings to his GP every year come from globalised sources. His medication sensitivity results come from Australia-based myDNA. The ECG records from AliveCor’s Kardia and his fitness activity from Fitbit comes from U.S. companies. The results from his microbiome test come from the U.K.’s Atlas Biomed. The list goes on.
Thanks to overseas companies that make their products and services available globally through online access and worldwide supply chains, Dr. Meskó is able to bring his personalised medical data to his GP in Hungary. By analysing these data, she was able to design a prevention program with diet and activity recommendations, and regular tests tailored to Dr. Meskó.
Such patients might not be the norm but soon will be, and physicians should also be adequately prepared. In order to better deal with this influx of international data, physicians should receive training in doing so. Medical schools’ curricula require updates in this regard, with a focus on digital health.
Moreover, regulations often lag behind the patient of the future. With digital health, the ivory tower of medicine is obsolete. As these technologies empower patients with their health data, they need an equal-level partnership in their care. The #wearenotwaiting movement from diabetics illustrates this. With the artificial pancreas not available on the market due to lagging regulations, the diabetics community designed their own DIY one that works. After two years since the DIY version became freely available, the FDA finally approved of an artificial pancreas.
The diabetics community illustrate the trojan horse of digital health, where empowered patients won’t wait for regulations to meet their needs. But this can be risky and new policies are necessary to better attend to patients’ needs in the digital health age.
Globalised policies
Without proper regulations from healthcare authorities, digital health tools can have harmful side effects unbeknownst to patients who adopt them. Recently, the fitness tracker company Garmin was the subject of a cyberattack which halted its services and put the users’ data in jeopardy. The company reportedly paid $10 million to liberate its systems. Amnesty International reported “serious security vulnerabilities” in Qatar’s mandatory COVID-19 contact tracing app. These could allow cyberattackers to access highly sensitive personal information such as names, national ID, health status and location data of over one million users. The contact-tracing apps of the U.K. and South Korea also had similar flaws.
These are only some of the recent examples where breach of private data was possible. Unfortunately, as adoption of these technologies happen on a larger scale, more of such instances will happen. As such, before digital health solutions are made available to consumers, the secure handling of data and quality of services offered should be ensured. The CE marking or even new rules have to be set up to ensure quality in both performance and data protection is offered.
Ultimately, a global FDA authority should be set up to address these issues brought forth by the globalisation of healthcare. Such an authority will be able to offer support to players in individual countries to solve global healthcare issues whether they are about wearables, smartphone apps, genetic testing or clinical trials.
Already, authorities took some steps in this direction. The World Health Organization (WHO) published its Global Strategy on Digital Health draft. It aims to support national or regional digital health initiatives so as to achieve “affordable and universal access to health for all”. The Global Digital Health Partnership, an international collaboration of 30 countries, states that its vision is to “support governments and health system reformers to improve the health and well-being of their citizens through the best use of evidence-based digital technologies”. Such initiatives are a must going forward in healthcare. They will help implement adequate policies for a globalised healthcare with the help of digital health.
Dr. Bertalan Mesko, PhD is The Medical Futurist and Director of The Medical Futurist Institute analyzing how science fiction technologies can become reality in medicine and healthcare. As a geek physician with a PhD in genomics, he is a keynote speaker and an Amazon Top 100 author.
Get access to exclusive content and analyses about the future of digital health on Patreon.com!
Subscribe here for The Medical Futurist newsletter to get exclusive details about digital health!