By Derek Yach, MBChB, MPH, Foundation for a Smoke-Free World
We conducted a survey in June of 2020 that addressed whether people’s willingness to use a COVID-19 vaccine and adopt other preventive healthcare measures was associated with trust
An effective COVID-19 vaccine could help us emerge from isolation and end the social distancing required during this pandemic; but it will only work if people are willing to be vaccinated [1].
We conducted a survey in June of 2020 that addressed whether people’s willingness to use a COVID-19 vaccine and adopt other preventive healthcare measures was associated with trust. The survey was conducted in nine countries: China, India, Indonesia, Italy, Japan, South Africa, Sweden, the United Kingdom, and the United States. A thousand individuals were surveyed in each country, and the responses were weighted to the most recent census data [2].
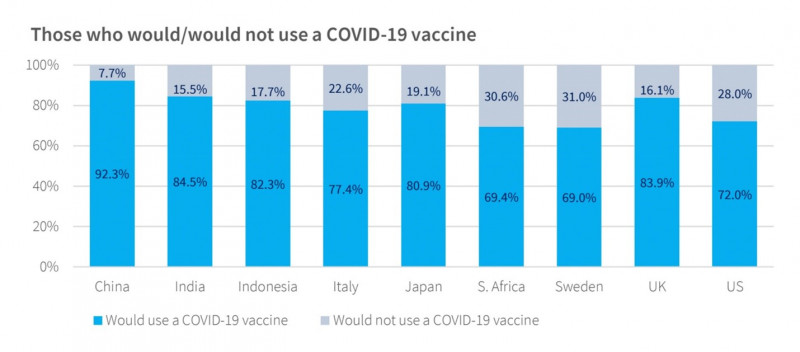
While an average of 86% of the respondents had increased the number of times they washed their hands in April and May of 2020, an average of 21% said that they would not get vaccinated. These figures were highest in Sweden (31%) and South Africa (30.6%), but were not much better in the United States (28%) and Italy (23%) (Figure A). Unfortunately, many of these levels barely reach the cusp of vaccine coverage needed to achieve population-wide herd immunity against COVID-19 [3], [4], [5].
Sources show that the public is most concerned with vaccine effectiveness and the risk of vaccine side effects [5], [6], [7], [8]. Worry about side effects has historically had a big influence on vaccine acceptance. In the UK, concern about reported neurological complications from common childhood vaccines lowered the vaccination rate from 81% in 1974 to 31% in 1980, leading to a resurgence of pertussis that resulted in over 100,000 cases [6]. In 2018, 20% of respondents to the Wellcome Global Monitor survey in the UK said they believed that the risk of vaccine side effects was fairly high or very high [7].
Interestingly, our survey showed that respondents who said they would get vaccinated had more education than those who said they would not get vaccinated. These results were highest in the U.S. and Sweden (Figure B). This may mean that people with more education have more information, but this correlation will need to be further explored before it can be explained.
Dr. Bruce Gellin, U.S. Deputy Assistant Secretary for Health and Director of the National Vaccine Program in the Department of Health and Human Services, has said that the foundation that underpins vaccination acceptance is trust [9]. Our survey explored respondents’ trust of both their national government and the medical profession (Figures C and D). With the exception of China, India, and Indonesia, most respondents had relatively low levels of trust in their national government, but most of the respondents said they trusted the medical profession. Trust in both entities, but especially in the medical profession, was generally higher among those who said they would get vaccinated. These findings emphasize the importance of having medical professionals lead messaging about vaccine safety, effectiveness, and benefits. [10] [11]
A recent piece in the Journal of the American Medical Association [12]on flu vaccination during the COVID-19 pandemic stated that strong, unified messaging is essential to vaccine compliance. The article cites the CDC’s call to action that urges physicians to make every effort to get their patients vaccinated and acknowledges that physicians and healthcare professionals are the most trusted source for accurate information on vaccine risks. The role of medical professions in preventing larger public health crises that could overwhelm the world’s healthcare resources cannot be overestimated.
We suggest that healthcare professionals partner with their national governments and international healthcare experts, such as the World Health Organization, to create consistent, accurate messages about the benefits of vaccination for COVID-19. These messages should use simple language that people with no more than an elementary education can understand; acknowledge peoples’ fears about vaccine side effects and cite accurate, verifiable data on side effect risks; and state whatever data is available on vaccine effectiveness. This will ensure that the greatest number of people will get vaccinated as soon as a vaccine is ready leading to a potential end to the current COVID-19 pandemic.
References
- [1] Swingle CA (2018) How Do We Approach Anti-Vaccination Attitudes? Mo Med 115:180–181.
- [2] https://bit.ly/2ZMwOCi
- [3] Dodd RH, Cvejic E, Bonner C, et al (2020) Willingness to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 14:484.
- [4] https://mayocl.in/3kuAxfE
- [5] Iboi EA, Ngonghala CN, Gumel AB (2020) Will an imperfect vaccine curtail the COVID-19 pandemic in the U.S.? Infect Dis Model 5:510–524. https://bit.ly/35MdyZB.
- [6] Larson HJ (2020) Stuck: How vaccine rumors start – and why they don’t go away. Oxford University Press.
- [7] Wellcome (2019) Wellcome Global Monitor 2018. 1–125.
- [8] Burki T (2019) Vaccine misinformation and social media. Lancet Digit Heal 1:e258–e259. https://bit.ly/2FGUocL.
- [9] Gellin B (2020) Why vaccine rumours stick—and getting them unstuck. Lancet 396:303–304. https://bit.ly/32HILLC.
- [10] Edelman (2020) 2020 Edelman trust barometer spring update: trust and the COVID-19 pandemic. In: Edelman. https://bit.ly/2FNZt2U.
- [11] Jamison AM, Quinn SC, Freimuth VS (2019) “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sci Med 221:87–94. https://bit.ly/2FJ92QN.
- [12] Jaklevic MC (2020) Flu Vaccination Urged During COVID-19 Pandemic. JAMA. https://bit.ly/3iJBFeW.